Receiving a diagnosis of end stage kidney failure in cats or chronic kidney disease (CKD) for your aging feline can be emotionally taxing. The overwhelming mix of worry, confusion, and anxiety can leave you seeking clarity and guidance on what lies ahead.
It’s imperative to recognize that a CKD diagnosis doesn’t mandate immediate euthanasia. Whether your cat is in the early stages or grappling with an advanced condition, comprehending how to assess your cat’s quality of life and effectively communicate with your veterinarian is paramount.
Understanding Feline Kidney Failure
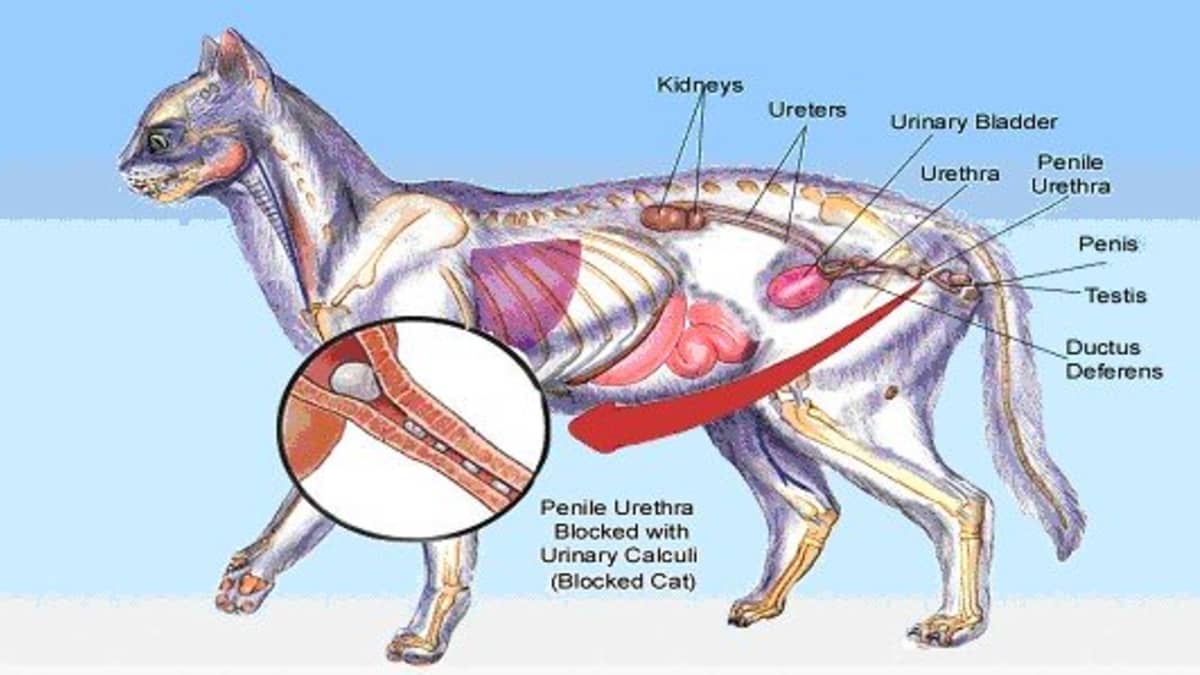
Kidney failure, often referred to as renal failure, arises from a variety of conditions affecting the kidneys and their interconnected organs. Normally, healthy kidneys perform several vital functions, including waste removal from the bloodstream, electrolyte balance maintenance, hydration and calcium regulation, blood pressure control, and stimulation of red blood cell production. When a cat experiences kidney failure, these critical functions falter.

Variations in Feline Kidney Failure
Two primary forms of kidney failure exist in cats, each differing significantly in causes, available treatments, and prognoses.
Acute Renal Failure: This rapid-onset kidney failure transpires within a brief span, typically days or weeks. It can affect cats of any age and often stems from toxic substances, disorders, diseases, organ malfunctions, medications, and various other factors. Timely intervention can sometimes reverse acute renal failure.
Chronic Kidney Failure: In contrast, chronic kidney failure leads to a gradual deterioration in kidney function over months or years. This deterioration gradually impairs the kidneys’ ability to eliminate toxins from the bloodstream and holds the potential to advance to complete kidney failure.
Unraveling the Causes of Feline Kidney Failure
Your cat’s kidney filtering system comprises thousands of microscopic tubes known as nephrons. While a damaged kidney can still function, a swift decline in too many nephrons—beyond the compensatory capacity of the remaining healthy nephrons—results in kidney failure.
The immediate fallout of kidney failure is the kidneys’ inability to effectively cleanse the blood of hazardous toxins. While kidney decline often correlates with age, cats aren’t exclusively susceptible. Several factors can trigger both acute and chronic kidney failure in cats:
Acute Kidney Failure:
- Ingestion of toxic substances (like toxic plants, antifreeze, rat poison, or human medications)
- Dehydration
- Bacterial infections, such as urinary tract infections spreading to the kidneys
- Illnesses like cancer
- Clotting disorders
- Low blood pressure (hypotension)
- Heart failure
- Blockages
- Specific medications (including some chemotherapy drugs or antibiotics)
- Trauma, such as a ruptured bladder or a broken pelvis
- Shock from excessive blood loss, overheating, vomiting, or diarrhea
- Chronic Kidney Failure
- Genetics
- Blockages
- Autoimmune diseases attack the body’s organs
- Cysts growing and impairing kidney tissues
Understanding the Telltale Symptoms of End-Stage Kidney Failure in Cats
When your feline companion’s kidneys struggle to eliminate waste effectively, they might exhibit several indications signaling kidney failure. Typical symptoms of kidney failure in cats encompass various facets:
- Weakness: Cats experiencing kidney failure often display a notable lack of energy and vigor.
- Weight Loss: Gradual or sudden weight loss can be a key symptom in affected felines.
- Lack of Appetite: A diminished interest in food or a complete loss of appetite can signify a problem.
- Depression: Cats may become withdrawn, uninterested, or exhibit altered behavior.
- Bad Breath: Foul breath can be a result of waste buildup in the bloodstream.
- Gastrointestinal Disturbances: Diarrhea or vomiting, potentially containing traces of blood, may occur.
- Dehydration: Reduced fluid levels may lead to symptoms of dehydration.
- Excessive Thirst: Cats may drink significantly more water than usual.

Besides these general indicators, acute kidney failure can manifest as an arched back or stiff-legged gait—a clear indication of potential pain caused by kidney issues. Conversely, signs of frequent or reduced urination can also denote a problem.
Recommended:
Understanding End-Stage Kidney Failure
The subtlety of chronic kidney failure progression may delay its detection. By the time overt symptoms arise, the disease may have significantly advanced. However, with timely intervention and suitable treatment, some cats can enjoy a good quality of life despite chronic kidney failure.
The symptoms of end-stage kidney failure in cats encompass a broader spectrum, often presenting as:
- Dull, Sunken Eyes: Eye appearance might change, reflecting the cat’s health decline.
- Mobility Challenges: Inability to walk or move comfortably.
- Odor: An unpleasant body odor can signal advanced disease stages.
- Incontinence: Inability to control urination or bowel movements.
- Seizures: Convulsive episodes can occur.
- Confusion: Behavioral changes might indicate neurological complications.
- Refusal to Eat or Drink: A clear sign of discomfort or pain.
- Twitching or Tremors: Muscle spasms or twitching might occur.
- Blindness: Visual impairment may manifest.
- Pacing and Restlessness: Agitated behavior might be observed.
- Withdrawal and Hiding: Seeking seclusion or running away.
Though not all symptoms may be evident, these indicators often coexist, highlighting the severity of the condition. Sudden fluctuations in symptoms should not mislead owners into assuming recovery.
Managing end-stage kidney failure necessitates diligent care and evaluation. Early diagnosis, continuous disease management, and effective communication with a veterinarian are pivotal.
For cats with this advanced condition, treatment aims to decelerate the ailment’s progression and alleviate discomfort. Approaches include intravenous fluids, nutritional support, potassium supplements, and medications to address nausea or vomiting.
In the final days of a cat’s life with end-stage kidney failure, maintaining a warm, comfortable environment with easy access to food, water, and litter, coupled with ample human companionship, is crucial.
Should your feline companion experience distressing symptoms like seizures or persistent vomiting, consult your vet about the possibility of euthanasia. While a heartbreaking decision, it’s essential to prioritize your pet’s comfort if other measures prove ineffective.
Understanding the Impact of Chronic Kidney Disease (CKD) in Cats: How It Alters Their Well-being
Cats’ kidneys play a vital role in their overall health—they act as intricate filtering systems, separating vital elements from waste in the bloodstream. A diagnosis of CKD in cats implies a disruption in this process. Veterinarians identify CKD when kidneys start accumulating waste materials and excreting essential substances that the body needs, reflecting in altered blood and urine analyses.
Initially, cats with CKD might exhibit minimal symptoms. However, signs eventually surface, often appearing as increased urine clumps in litter boxes or alterations in appetite leading to weight loss. Some may encounter vomiting, diarrhea, or gastrointestinal issues. Laboratory tests usually confirm the diagnosis when examining samples.
To assess the severity of CKD, a system known as IRIS (International Renal Interest Society) staging assists veterinarians in plotting suitable treatment pathways and predicting outcomes at each disease stage.
Consulting with your veterinarian about the IRIS staging can elucidate your cat’s current condition and offer insights into the potential course of the disease.
Life Expectancy and CKD
The prognosis for cats diagnosed with CKD varies significantly based on the disease stage and the chosen treatment plan. Cats in the early stages of CKD who receive dedicated care can often live for years. In some remarkable instances, with attentive management, cats have thrived for over a decade.
However, the life expectancy factors in the overall health of the cat and potential concurrent organ dysfunctions. Older cats with multiple health issues may face shorter lifespans, but diligent care might extend their lives for 2-3 years or more.
It’s not uncommon for aging cats to have CKD coupled with conditions like an overactive thyroid or hypertension. While none of these diseases result in immediate fatality, they do add complexities, demanding comprehensive care for stabilization and restoring comfort.
On the flip side, cats diagnosed in advanced CKD stages or residing in situations where treatment isn’t viable usually face shorter lifespans—sometimes merely weeks to months.
Following diagnosis, discussing treatment options promptly is crucial. This phase demands the most assertive approach in caring for your cat’s health.
When to Consider Euthanasia
Deciding on euthanasia for a cat grappling with CKD presents a complex emotional challenge, particularly after investing heavily in treatment. At times, caregiver fatigue clouds judgment, prompting a reevaluation of the situation, which becomes necessary.
Sometimes, an outsider’s perspective—a visiting family member or friend—reveals the substantial changes in your cat’s condition or the intensity of care needed, leading to a rethinking of choices. Approaching this decision often involves looking at the world through your cat’s eyes and assessing their quality of life (QOL).
In human medicine, conversing with a patient aids in treatment adjustments, but with cats, it’s reliant on interpreting nonverbal cues—body language and behavior. Evaluating your cat’s QOL becomes essential.
Assessing Your Cat’s Quality of Life
The core consideration revolves around gauging your cat’s pleasure in routine activities. Even amid fluctuating good and bad days, observing whether they relish meals, enjoy basking in the sun, or engage in cherished interactions helps evaluate their contentment.
Creating a list of your pet’s usual joys and using a ranking system from 1-10 on a calendar for each day aids in tracking patterns. A consistent trend of scores from 7-10 might suggest a content cat. Scores dipping to 5-7 signal growing concerns, while scores consistently below 5 demand deliberation on difficult decisions.
Here are some specific areas to consider:
Appetite: Although many kitties with CKD are prescribed a prescription diet as part of their protocol, at some stages, it becomes important to just keep them eating.
- Is your cat eating enough to maintain a stable weight?
- If they are losing weight, how quickly is it dropping?
- Do they still enjoy eating, even if they may be picky?
- When you break out the “good stuff,” like some roast beef or a can of tuna, does that spark some interest?
- Are you able to get calories in, even if you need to give your cat an appetite stimulant?
Attitude: Pay attention to your cat’s daily routine, attitude, and behaviors.
- What’s your cat’s daily routine? Is it close to what it was a year ago? Do they get up, have a snack, use the litter box, and go back to bed for several hours? Or is your cat uncomfortable and pacing or restless?
- Does your cat sleep all day long without any interest in getting up to follow the sun as it moves about the house?
- Does human interaction seem enjoyable? Playtime might be a lot to ask, but willingness to play is a big plus in the quality of life column.
- Are grooming sessions as enjoyable as they once were, or are they starting to seem painful? Many cats with CKD start to have difficulty getting on and off furniture as they lose muscle mass, but do they still have the desire to get on the couch and the forbidden kitchen table?
Medications: Most cats with CKD will wind up on medications, which vary with the stage of the disease. With some cats, this can be multiple medications, such as subcutaneous fluids, phosphorous binders, electrolyte supplements, and special diets, amongst others. If they have other diseases, even more medications may be involved. Judging how well your patient tolerates the daily stress of treatment is an important factor.
- How stressful is the process of giving medications to your cat? Can it be tweaked or streamlined? Although it sounds extreme, some cats even benefit from a feeding tube. This allows you to provide calories and medications all at once with minimal stress and can be hugely life-extending for some cats.
When you notice that these basic categories are starting to consistently drop to a level that indicates that your kitty isn’t happy with life anymore, it’s time to consider euthanasia.
As these categories begin consistently trending downwards, indicating diminished happiness, the contemplation of euthanasia becomes inevitable.
Recognizing End-Stage CKD
In advanced CKD stages, signs indicating your cat’s declining health include:
- Reduced appetite unresponsive to stimulants.
- Rapid weight loss.
- Excessive drinking and urination, possibly leading to a complete cessation.
- Episodes of vomiting, diarrhea, or mouth ulcerations.
These noticeable drops in QOL serve as crucial indicators, signaling the impending decision.

Palliative Care, Hospice, and Euthanasia
Following a CKD diagnosis, palliative care becomes the immediate approach for cats in early-middle disease stages. This phase entails formulating a plan aimed at minimizing disease progression while ensuring the best QOL.
As CKD progresses, transitioning to the hospice stage focuses on maximizing comfort rather than extending life. Catering to your cat’s comfort becomes paramount, even if it means compromising treatment duration for improved quality.
Finally, when hospice care struggles to sustain your cat’s QOL, considering euthanasia becomes inevitable, albeit distressing. Consulting your veterinarian for advice, evaluating treatment efficacy, and discussing after-care options are essential preparatory steps.
Note: The advice provided in this post is intended for informational purposes and does not constitute medical advice regarding pets. For an accurate diagnosis of your pet’s condition, please make an appointment with your vet.
References
- Polzin DJ. “Chronic Kidney Disease in Small Animals.” The Merck Veterinary Manual. Merck Sharp & Dohme Corp., 2019. [Online]. Available: https://www.merckvetmanual.com/urinary-system/noninfectious-diseases-of-the-urinary-system-in-small-animals/chronic-kidney-disease-in-small-animals.
- Syme H. “Diagnosis and Management of Feline Chronic Kidney Disease.” Journal of Feline Medicine and Surgery. 2013. 15(7): 631-42. DOI: 10.1177/1098612X13484100.
- IRIS (International Renal Interest Society). “IRIS Staging of CKD.” IRIS Kidney. [Online]. Available: https://www.iris-kidney.com/guidelines/staging.html.
- Bartges J. “Chronic Kidney Disease in Dogs and Cats: Perspectives on Diagnosis, Management, and Prognosis.” Veterinary Medicine: Research and Reports. 2014. 5: 257–66. DOI: 10.2147/VMRR.S44451.
- Chew DJ, et al. “Chronic Kidney Disease in Cats.” ACVIM Consensus Statements: Guidelines for the Identification, Evaluation, and Management of Systemic Hypertension in Dogs and Cats. 2018. 1-14.
- Chakrabarti S, Syme HM, Brown CA, Elliott J. “Histomorphometry of Feline Chronic Kidney Disease and Correlation with Markers of Renal Dysfunction.” Veterinary Pathology. 2013. 50(1): 147-55. DOI: 10.1177/0300985812447437.
- Sparkes AH, et al. “Chronic Kidney Disease in Cats: UK Guidelines for Identification, Diagnosis, and Management.” Journal of Feline Medicine and Surgery. 2016. 18(3): 219-39. DOI: 10.1177/1098612X15585027.
- Ross SJ, et al. “Evaluation of the Association between Initial Proteinuria and Morbidity Rate or Death in Cats with Chronic Kidney Disease.” Journal of the American Veterinary Medical Association. 2013. 243(12): 1710-19. DOI: 10.2460/javma.243.12.1710.
- Scherk M, Laflamme D. “Nutritional Management of Chronic Kidney Disease in Cats & Dogs.” Veterinary Clinics of North America: Small Animal Practice. 2016. 46(6): 1015-30. DOI: 10.1016/j.cvsm.2016.06.005.
- Elliott J, Syme H. “Reassessment of Treatment of Chronic Kidney Disease in Cats.” Veterinary Record. 2019. 185(3): 70. DOI: 10.1136/vr.l6238.
